By C. Todd Lopez
WASHINGTON (Oct. 10, 2017) -- "It's one of the least dramatic tests you'll ever see. You hit start, you go get coffee, maybe lunch, come back and download the file," said Jack Norfleet at the Army Research Laboratory.
What Norfleet and a summer intern in his lab were actually doing was using a piece of precision equipment to slowly stretch to the point of breakage a small piece of artificial material that might one day stand in for human tissue on medical training devices.

Norfleet said that Soldiers in the Army's medical community regularly train on simulators -- mannequins and dummies that look like real people -- to practice critical lifesaving skills such as hemorrhage control, needle chest decompression and airway management.
Those dummies, he said, are meant to simulate the human body as closely as possible. But they are not real humans, just simulators. They use rubber and plastic as analogues for skin and bone and other tissues found in the human body. But they are not always spot-on in mimicking how the human body actually behaves, Norfleet said. And that can be a problem for Soldiers who need the most accurate training possible.
One type of tissue that needs a better stand-in on medical dummies is the human pleura, Norfleet said. To explain what the pleura is, he referenced a rack of barbeque ribs.
"You know that real clear tough membrane on the inside? That's the pleura," he said.
Humans have a pleura lining their own ribs. And Soldier medics will encounter the pleura when treating a collapsed lung, or "tension pneumothorax," Norfleet said.
"It means there's air around the lung, it builds up pressure, and the lung cannot expand," Norfleet said. "It's the second-most common preventable killer on the battlefield. It doesn't have to be a sucking chest wound, but a sucking chest wound will create a tension pneumothorax. It could be a close blast injury, or even an impact in a car accident."
When medics need to treat a collapsed lung, they might have to drive a needle between the patient's ribs, pushing through the pleura, to create a path for air and fluid that's trapped between the lung and chest wall to escape.
In training and in real life, Soldiers will know they've made it through the pleura when they feel the needle "pop" through that tissue. They have to be skilled at knowing where to place the needle, how far to push the needle in, and how hard to press the needle into the patient.
On a training dummy, having all those factors correct is not so important, because the dummy can't be injured. But on a real Soldier, incorrect placement of the needle, or pushing it in too far can be life-threatening.
"If you are in the wrong place, you can hit a nerve bundle, or you can hit a major vessel," Norfleet said.
So training for Soldiers on dummies is important. And ensuring those dummies simulate human tissue as closely as possible is also important, he said.
A real human pleura, Norfleet said, breaks at about 2 megapascals, and can stretch to about 1.7 times its original length. The material that simulates the pleura, on modern-day training dummies, however, doesn't accurately simulate that.
"It breaks at 14 megapascals, and stretches at three times as long," he said.
Those dummies, he said, have been used to train "over a million medics."
"We're training them to drive a nail with a sledge hammer, when what they need is a detail hammer," Norfleet said.
Norfleet said that Soldiers who aren't aware of the difference between how much pressure they apply in training, versus how much pressure they should actually apply on a real human, might do more harm than good -- pushing their needle all the way into the lung, he said, which will "make the problem worse."
He said the Army, and the researchers at ARL, would like to find better materials to use in training dummies so that when medics actually perform procedures on real Soldiers in the field, their experience there is as close as possible to what they saw while training on the dummies.
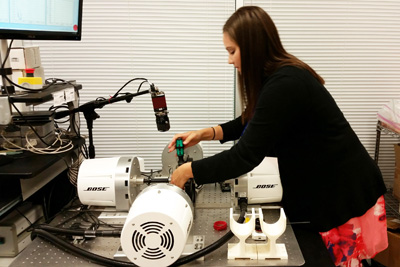
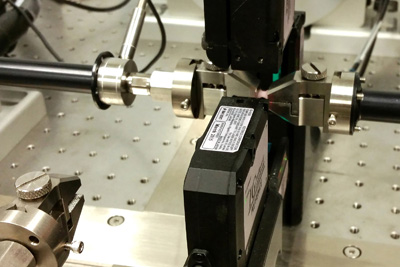
At ARL-Orlando, Norfleet is testing various types of rubbers and other artificial materials to see how far they can stretch before breaking, and what it takes to puncture them. It's part of an effort to document the properties of various materials that might be used in training dummies and other medical simulators.
While in Orlando they test only artificial tissues, similar testing on actual human tissue is being done elsewhere.
"We have an exact duplicate of this test up at the University of Minnesota, and another at the University of Washington," he said. "They are taking the human tissues from donors and running the exact same tests."
What Norfleet can do then is use test data from an actual human pleura, and then using his own tests, try to find suitable artificial materials that will mimic it for use in training simulators.
In addition to finding suitable stand-ins for human pleura, they are also looking at substitutes for airway tissues, the fascia and lower-leg tissues, among other things, he said.
The testing that Norfleet is doing in Orlando, coupled with the testing done on actual human tissue, will eventually yield better physical training simulators for Soldiers.
But the work benefits more than the dummies. It will also benefit robotic-aided surgery and virtual simulators as well. Both require accurate information on how human tissues behave, so that they can, for instance, provide accurate haptic feedback to a surgeon who might be doing surgery with a robotic arm rather than his own hand.
"We think the application [of our work] is much greater in virtual simulations, because more and more procedures are being done with laparoscopic or robotic tools," Norfleet said. "So the human hands on the body during surgery is going to start to become rarer. And the tools in the body surgical procedures are becoming more prevalent. So the virtual trainers, where you never actually touch the tissue, are going to be the higher demand area. If you are programming grasping a polyp in a colon and pulling it with a certain amount of force, this data will tell you how much it stretches and how much force it's putting back against you and also when it will tear."